A Guide to Patient Positions in Medical Beds
I believe that positioning patients correctly in medical beds is key to giving the best care. From my experience, the right position helps a patient feel more comfortable and safe. It also makes medical treatments work better. Good positioning keeps the body in a straight line. It helps the body work as it should and lowers the chance of health problems. This is the adjustable posture of a multi function electric hospital bed produced by Grace Medy Hospital Bed Manufacturer:
Common Patient Positions in Medical Beds
From my experience, getting a patient’s position on adjustable medical bed right is key for their care and safety. Here are some of the main positions in medical beds. Each position has a specific medical purpose, with its own benefits and things to watch out for.
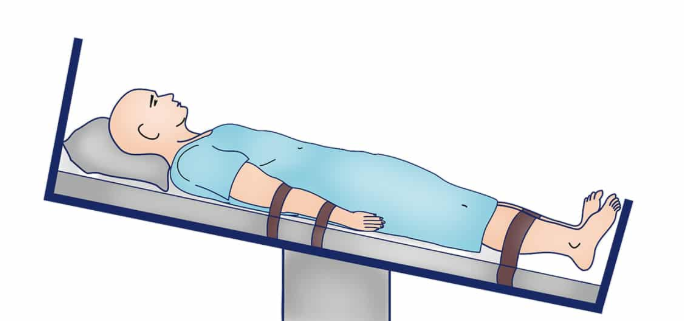
Supine Position (Flat on Back)
What it is: Patient lies flat on their back, looking up at the ceiling. Head might be flat or on a small pillow. Arms are down by their sides or resting on their belly; legs are straight out (a pillow under the knees can help some people).
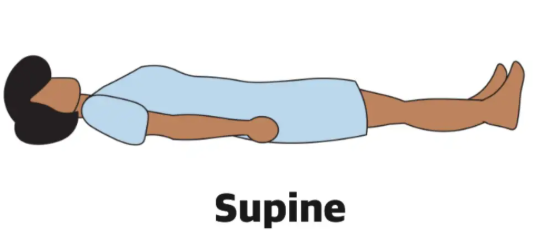
Why it’s used: The basic position for check-ups, taking temperature/blood pressure, waking up after surgery, getting IV fluids, and many operations (like on the belly or chest). Also used for resting or sleeping.
Why it helps: Very stable. Makes it easy for staff to check the front of the body. Keeps the spine straight.
Things to watch: Can cause sore spots on the back of the head, shoulder blades, tailbone, and heels if lying too long. Can make back pain worse. Not great for people having trouble breathing, severe heartburn, or who might choke. Needs regular position changes.
Fowler’s Position (Sitting Up in Bed)
What it is: The head of the medical bed is raised so the patient sits up. Knees can be slightly bent for comfort.
Different Heights:
Slightly Up (30-45°):Good for people who might choke (like on tube feeds), mild breathing trouble, or after belly surgery.
Halfway Up (45-60°):Best for easier breathing, eating, talking, or moderate breathing problems.
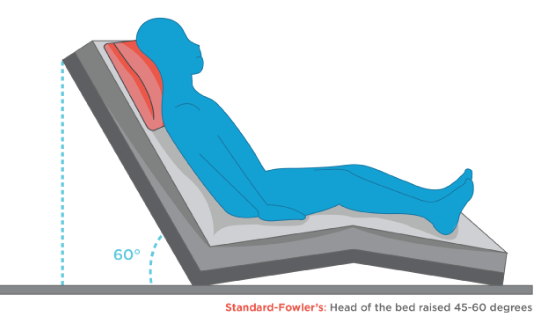
Mostly Upright (60-90°):Used for serious breathing trouble (like bad COPD or lung fluid), swallowing problems, or to reduce head swelling.
Why it’s used: Helps people breathe easier, swallow safer, prevents choking, feels better after chest/belly surgery, reduces face/neck swelling.
Why it helps: Takes weight off the lungs so they can expand better. Lets mucus drain easier. Makes swallowing work with gravity. More comfortable for being awake.
Things to watch: Patient can slide down the bed (use footrests or leg pillows). Can put pressure on the tailbone. Back needs support. Check skin on tailbone and heels.
Tripod Position (Sitting and Leaning Forward)
What it is: Patient sits bolt upright, either in bed or on the edge, and leans forward, resting on a table with pillows, their knees, or stacked pillows. Elbows are bent.

Why it’s used: Serious, sudden breathing trouble (like bad asthma attacks, COPD flare-ups, heart failure with lung fluid).
Why it helps: Makes the most space for lungs to fill with air. Lets the patient use neck and chest muscles to breathe. Helps cough up mucus. Takes some pressure off the heart.
Things to watch: Patient needs help getting into position and might get tired quickly. Needs someone nearby. Support must be sturdy. Not for people who are passed out or very weak.
Prone Position (Flat on Stomach)
What it is: Patient lies flat on their belly, face turned sideways (using a special face pillow with a hole). Arms can be by sides, bent up near head (“swimmer”), or on pillows. Chest and hips propped slightly; toes might hang off the bed.
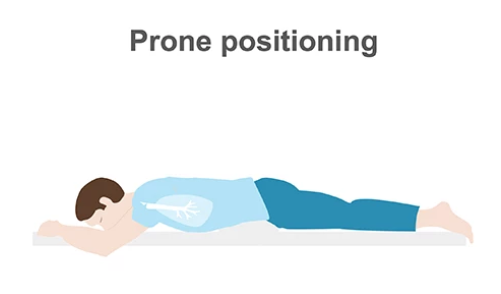
Why it’s used: Serious lung failure (like bad COVID on a breathing machine), some back surgeries/treatments, wounds on the back, or when oxygen levels are dangerously low.
Why it helps: Helps get oxygen into the blood better in sick lungs. Makes it easier to cough up mucus from the back of the lungs. Takes pressure off the tailbone and heels.
Things to watch: Turning requires a special team (risks pulling out tubes or hurting the neck). Needs constant watching of breathing, tubes, and skin. High risk for sore spots on face, chest, hip bones, knees, and feet. Head must be turned often. Eyes need protection. Not for: People with neck/back injuries, some face/chest injuries, unstable blood pressure, or pregnant women.
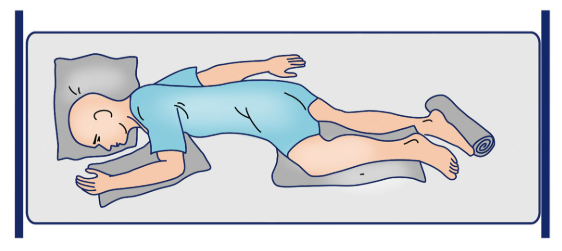
Lateral Position (Lying on Side)
What it is: Patient lies on their left or right side. Body straight. Head level. Bottom arm out front or behind; top arm rests on a pillow or the bed. Top leg bent, knee resting on a pillow. A pillow behind the back helps.
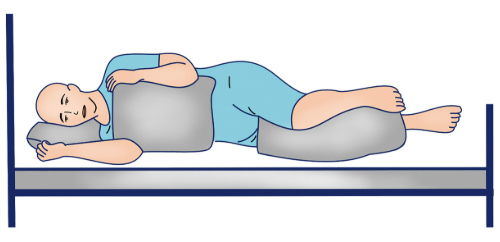
Why it’s used: Prevents bed sores by shifting weight. Regular turning schedule for bed-bound patients. Helps drain mucus from specific lung areas. Comfortable for sleeping. Used for some tests (like back taps). Safe position for unconscious people (prevents choking).
Why it helps: Takes pressure off the tailbone and heels. Helps clear the bottom lung. Often feels comfortable.
Things to watch: Keep body straight to avoid strain. Pillow MUST go between knees/ankles and under top arm. Avoid pressure on the bottom shoulder and ankle bone. Turn patient regularly (e.g., every 2 hours). Check skin on hip bones, ribs, knees, ankles.
Trendelenburg Position (Head Down)
What it is: Whole bed tilted so head is lower than feet (about 15-30°). Patient is still flat on back.

Why it’s used: Debated for severe shock (to try getting more blood to heart); certain surgeries (belly/pelvic – moves organs up for better view); quick placement of a big chest IV line.
Why it helps: In theory, gravity pulls blood towards the heart. Helps surgeons see during some operations.
Things to watch: Big Risks: Raises pressure in the head and eyes, makes breathing harder. Causes face/head swelling. Nausea/heartburn. Avoid in: Head injuries, strokes, high head pressure, glaucoma, breathing/heart problems. Use is rare and risky.
Reverse Trendelenburg Position (Head Up)
What it is: Whole bed tilted so head is higher than feet (about 15-30°). Patient is still flat on back.
Why it’s used: After brain/neck/weight-loss surgery. To lower head pressure. Helps breathing if sitting fully up isn’t possible. Used in some upper belly surgeries. Reduces heartburn.
Why it helps: Lowers pressure/swelling in the head and face. Takes some weight off the lungs. Uses gravity to keep stomach acid down. Gives surgeons better access.
Things to watch: Patient can slide feet-first down the bed (use footrests/knee supports). Puts more pressure on tailbone/heels. Make sure patient is secure. Watch for low blood pressure.
Sims’ Position (Halfway on Side/Stomach)
What it is: Patient lies mostly on left side. Left arm stretched behind. Right arm bent near head. Right knee pulled up towards chest. Left leg slightly bent. Chest tilted slightly down towards the bed.
Why it’s used: Rectal exams, inserting suppositories/enemas, short colon checks. Cleaning the pelvic area. Safer position for sleepy/unconscious patients. Comfortable for some (like pregnancy). Helps clear the right lung bottom.
Why it helps: Easy access for rectal care. Safer for breathing than flat on back. Takes pressure off tailbone and hips.
Things to watch: Don’t trap the bottom arm underneath. Support the top bent leg well. Might be hard for people with hip/knee pain. Check skin on front hip bone and outside knee.
Summary
Based on my experience in healthcare, I’ve learned that good patient positioning is more than just following a checklist. I believe it’s about seeing what each person truly needs. Every time we move a patient, it matters greatly. A small adjustment on medical bed can mean they feel comfortable instead of having pain. It can help them heal or stop other problems from starting. As caregivers, I feel it is our duty to make patients feel safe and cared for. The things we learn today help us give better care tomorrow, one small move at a time.
