Supine Position
Think of the supine position as the “default” setting in healthcare. It is the most comprehensive resting posture: the patient lies flat on their back, facing the ceiling, with the head, neck, and spine aligned in a neutral straight line. On a medical bed, this essentially means the mattress deck is completely horizontal. While it looks simple, proper execution on a hospital bed often involves small, critical adjustments—such as placing a thin pillow under the head to prevent neck strain, or positioning a roll under the knees to relax the abdominal muscles and reduce pressure on the lower back.
Clinical Applications on Medical Beds
This position serves as the foundation for a vast number of medical procedures. It is the primary choice when doctors need access to the anterior (front) part of the body. In surgical contexts, the medical bed works as a stable platform for operations involving the abdomen, heart (thoracic), face, or neck. Beyond the operating room, it plays a crucial role in daily care:
Critical Examinations: Nurses and doctors use this position to palpate the abdomen or listen to heart and lung sounds without obstruction.
Post-Anesthesia Recovery: After surgery, keeping a patient supine ensures steady blood flow to the brain while they wake up.
Diagnostic Imaging: Almost all X-rays, CT scans, and MRIs require the patient to lie flat to get clear, standard images.
Prone Position
Flip the patient face-down. This opens access to the entire back anatomy. The patient lies stomach-down with their face turned to one side. Keep the hips straight—no flexing. Place support pillows under the head and legs. This keeps proper alignment and reduces pressure on sensitive areas.

Surgical Applications and Clinical Uses
Back surgeries make up most prone position cases. Spine procedures need direct back access. This makes the position essential. Hip surgeries use this setup too. Surgeons need it to reach the back of the joint. Rectal procedures work well in prone position. You get clear visibility and working space. Brain surgeons pick this position for certain cases. They need access to the back of the skull. Adrenal surgery may need it as well. It depends on the surgical approach.
Prone positioning helps outside the operating room too. Switching patients between back-down and face-down stops pressure sores. This prevents them from forming on the same spots. Breathing therapists use prone therapy. It helps breathing in some lung conditions. After surgery, care plans include prone positioning. This aids healing and drainage for certain procedures.
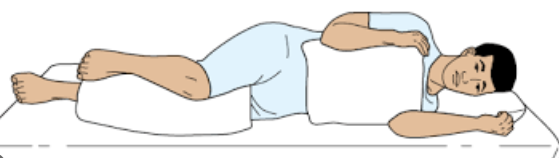
Lateral Position
The patient lies on their side. The body turns about 90 degrees from lying flat on the back. The top leg crosses over the bottom leg. Both hips and knees stay bent. This creates a stable side-lying position on the bed. Pillows make this position work well.
Place one pillow under the head and neck. This keeps the spine straight. Put another pillow between the knees. This stops pressure points and keeps the hips and knees bent. A rolled blanket or pillow goes behind the back. This keeps the patient from rolling backward. The upper arm needs support. A pillow under it stops shoulder strain during long periods in this position.
Medical Uses and Position Types
Lateral positioning helps with many medical needs. Surgeons doing back and hip operations use this setup. It gives them direct access to the surgical area. The position takes pressure off the tailbone and lower back. Patients healing from injuries in those areas need this relief. Doctors use lateral positioning after some surgeries. It helps with healing and drainage. Patients who struggle to breathe benefit from this position. Standard positions sometimes don’t help enough.
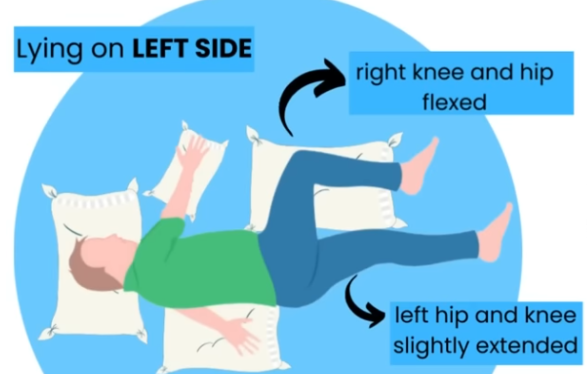
This position has specific types. Right lateral positioning means the patient lies on their right side. Most cases use this as the standard setup. Left lateral positioning is the opposite. The patient lies on their left side. Doctors pick this option to protect or treat the right side. Semi-lateral positioning is also called Sims’ position. The patient lies between back-down and face-down. The legs stay bent. Doctors use this type often for gynecologic and rectal exams.
Sims Position
Sims position puts the body at a diagonal angle. It mixes side-lying and face-down positions. The lower body rests on one side. The upper body tilts forward toward the bed. The lower arm goes straight behind the back. The upper arm bends at the shoulder and elbow. It rests in front of the body. The upper leg bends more than the lower leg. This diagonal torso angle is what makes this position unique.
Medical Applications and Procedures
Medical teams use Sims position for specific exams and treatments. Rectal exams work best this way. Doctors get clear access to the anal and rectal areas. Patients don’t need to twist into difficult positions. Nurses use this setup to give enemas. Gravity helps the procedure work. Patients stay comfortable too. Gynecologists pick Sims position to check for vaginal wall prolapse. They can see the posterior vaginal wall clearly.
Sigmoidoscopy works well in this position. Some patients can’t handle the knee-chest position. Joint problems or mobility issues make certain positions too hard for them. Sims position gives them another option. Post-surgery care often includes this position. It helps the body heal. It also keeps patients comfortable during recovery.
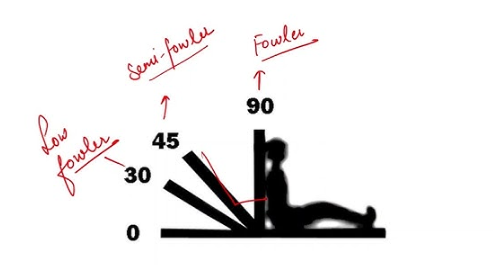
Fowler’s Position
Raising the head of the medical bed changes patient comfort and clinical results. Fowler’s position lifts the head of bed between 45 and 60 degrees. This creates a semi-sitting pose that serves many medical needs. Three variations exist to match different patient needs and treatment goals.
Low Fowler’s raises the bed just 15 to 30 degrees. This gentle lift works for patients who need mild support without full sitting. Semi-Fowler’s lifts the head 30 to 45 degrees. This middle range balances comfort with healing benefits. High Fowler’s pushes the angle to 60-90 degrees. The patient sits almost vertical in this steepest form.
Breathing Support
The raised position improves how patients breathe. Chest expansion reaches its fullest when the upper body rises. The diaphragm drops lower into the belly. The lungs get more room to fill with air. Gravity pulls the belly organs downward. They stop pressing against the chest. Belly muscle tension drops to low levels. The chest wall faces less push from gravity in this angled position.
These changes boost oxygen levels in the blood. Patients with mild to moderate breathing problems feel relief. The lungs work better without fighting against tight space. Air moves in and out with less effort. Medical teams use this position for patients healing from chest surgeries. It also helps those with pneumonia, COPD flare-ups, or heart failure affecting breathing.
Digestive System Benefits
Fowler’s position helps the digestive tract work better. Belly muscles relax fully in this setup. Digestion gets easier with loose stomach muscles. Food moves through the system with more ease. Gravity pulls everything downward through the digestive path. This natural pull speeds up peristalsis—the wave-like muscle movements that push food along.
Swallowing works better at raised angles. Patients using feeding tubes face lower choking risk. The upright angle stops fluids from flowing backward into the lungs. Food and liquids travel down toward the stomach instead of up toward the airways.
Orthopneic/Tripod Position
Some patients can’t breathe well sitting up in bed. They need a setup that opens the chest more than standard Fowler’s. The orthopneic position seats the patient upright at the bed’s edge with an overbed table placed in front. Pillows stack on the table. The patient leans forward onto these pillows for support and rest. This creates a tripod shape with the body—arms and trunk form the structure that gives more breathing space.
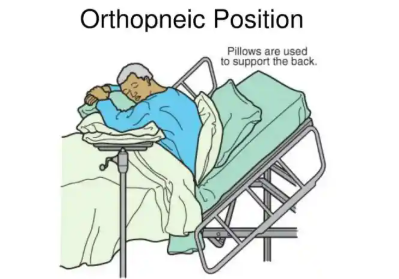
Better Breathing Support
This position gives the most chest expansion possible in a medical bed. The chest cavity reaches full volume as the trunk leans forward onto the table. Belly muscles release all tension in this pose. Gravity stops pulling against the chest wall. The diaphragm drops to its lowest point. The lungs gain maximum room to fill with air. Oxygen levels climb. Breathing becomes easier.
Patients who struggle to breathe out get special help from this position. They can press the lower chest against the table edge. This pressure helps with breathing out. Air moves out of the lungs with less effort. Patients with blocked airways benefit most from this breathing aid.
Clinical Uses
Medical teams use orthopneic positioning for breathing emergencies and ongoing breathing problems. Patients with moderate to severe breathing trouble need this setup. Standard positions don’t give enough relief. Those with breathing out problems or blocked airways need the extra chest expansion. Heart failure patients who develop fluid in the lungs shift to this position once lying down becomes too hard. The forward-leaning pose with arm support cuts down the work of breathing during distress.
Trendelenburg Position
Lower the bed head below the feet. Tuck the patient’s arms close to their sides. This inverted setup shifts gravity and moves blood toward the chest and head. The angle runs from 15 to 30 degrees. Clinical needs and patient comfort determine the exact tilt.Multifunctional five-function medical beds typically possess this function.With the control of the motor or crank, the adjustable medical bed will tilt to form the Trendelenburg position or the Reverse Trendelenburg position.

Emergency Medical Uses
Medical teams use Trendelenburg during critical situations. Low blood pressure and shock are the main reasons. The head-down angle pushes blood back to vital organs. The heart gets more blood volume to pump. The brain receives better blood flow during emergencies. Venous return increases in this position. Gravity pulls blood from the lower body toward the chest and head.
Surgical teams use this position during pelvic and lower belly procedures. The intestines shift upward and away from the surgical field. This creates clear workspace for the surgeon. Laparoscopic surgeries benefit from this organ shift.
Safety Monitoring Requirements
Close watching prevents problems from this inverted position. Patients with head injuries need extra care. The head-down angle raises pressure inside the skull. Brain swelling becomes more dangerous in this setup. Medical staff check brain pressure readings often during use.
Patients often slide toward the head of the bed in this tilted position. Proper straps stop this movement. Safety belts and positioning aids keep the patient stable. Healthcare teams check patient comfort throughout the procedure. Some patients struggle with the inverted feeling and breathing changes.
Reverse Trendelenburg Application
Flip the angle for digestive system problems. Reverse Trendelenburg raises the head above the feet. Stomach acid stays down in this elevated setup. Patients with severe acid reflux get relief from this position. Food and digestive fluids face gravity pulling them away from the throat. The risk of choking drops during meals and tube feedings.
Reverse Trendelenburg Position
Tilt the entire bed frame so the head rises 30 to 45 degrees above the feet. The whole bed slants upward from foot to head—not just the head section bending up like Fowler’s position. This tilt affects the body in special ways. Standard head-raising positions can’t do this. The patient’s body stays straight along the bed’s angle. No bending at the waist or hips. The spine stays aligned. Gravity pulls on the body in a new way.
Digestive System Protection
Reverse Trendelenburg stops stomach contents from flowing backward. Gravity fights acid reflux for you. The raised upper body keeps digestive fluids in the stomach. Patients with severe GERD get relief from this setup. The upward tilt stops nighttime reflux. This protects sleep and prevents throat damage. Medical teams use this position for tube-fed patients too. Food stays in the digestive tract. It won’t creep back toward the lungs. Aspiration risk drops during feeding times.
Breathing and Blood Flow Benefits
Critical care units switch between reverse Trendelenburg and standard Trendelenburg. Moving between these tilts keeps blood pressure stable in patients with weak hearts. The gravity changes help the heart pump better. Blood flow shifts with each position change. This approach helps patients whose hearts can’t pump well.
The semi-recumbent version lifts the head up to 45 degrees. ICU nurses use this angle to stop ventilator pneumonia (VAP). Patients on breathing machines face serious infection risks. The raised chest stops fluids from pooling in the lungs. Breathing gets easier as the chest expands. The diaphragm drops lower. Belly organs don’t push upward. Air moves in and out with less effort.
Patient Safety Monitoring
Nurses check skin contact points every two hours. The tilt shifts body weight in new patterns. Pressure hits different areas than flat or Fowler’s positions. Heels and lower back need extra padding. Staff check these areas often. Healthcare teams watch breathing patterns. Some patients find the slant hard to get used to. Vital signs show how well each patient handles the position.
